Healthcare APIs have come a long way — from nice-to-have technical tools to must-have infrastructure. These digital bridges are changing the game in how organizations connect their systems, share critical data, and ultimately deliver better patient care. But let's be honest: building APIs that actually work in healthcare isn't simple. You've got to juggle everything from tight security protocols to tricky interoperability standards.
Today, we'll dig into what really matters when building healthcare APIs — those make-or-break considerations that separate successful implementations from costly headaches. Get these right, and you'll create solutions that actually move the needle on patient care while checking all those compliance boxes.
- Decoding the Purpose: What Healthcare APIs Really Do
- Beyond the Basics: Real-World Impact of APIs in Healthcare
- Essential Building Blocks: Core Functionality Every Healthcare API Needs
- Critical Success Factors: Make-or-Break Considerations for Healthcare APIs
- Speed and Reliability: Performance Strategies That Actually Work
- Patient-Centered Design: How APIs Transform Care Delivery
- Overcoming Obstacles: Solutions to Common API Roadblocks
- Looking Forward: Emerging Technologies Reshaping Healthcare APIs
- Implementation Playbook: Best Practices for Healthcare API Success
- Building the Connected Healthcare Ecosystem
Decoding the Purpose: What Healthcare APIs Really Do
Before diving into implementation details, it's crucial to understand what healthcare APIs are actually designed to accomplish. These digital connectors serve specific purposes that directly impact patient care and organizational efficiency.
Healthcare APIs serve as vital intermediaries that process data transfers between diverse healthcare systems. At their core, these APIs function as translators and exchangers, enabling communication between different applications and databases that would otherwise remain isolated silos of information.
Think of healthcare APIs as the nervous system for your digital health setup—they're constantly firing, transmitting vital information across your healthcare environment, making sure the right data gets to the right place at the right time. No small feat in healthcare!
Beyond the Basics: Real-World Impact of APIs in Healthcare
The magic of well-implemented healthcare APIs isn't in their code—it's in their results. Patients receive better care, providers spend less time battling systems, and healthcare organizations run more smoothly. These aren't just technical upgrades—they're game-changers that reshape how healthcare actually works on the ground.
Transforming Healthcare Data Exchange
The primary function of healthcare APIs is to streamline the sharing of patient information across different providers. By establishing these digital pathways, organizations can enable real-time access to clinical information for both patients and healthcare professionals, breaking down the walls that have traditionally separated healthcare data.
This transformation isn't just technical—it's fundamentally reshaping how healthcare information flows throughout the entire ecosystem.
Enhancing Patient Care Through Connectivity
Healthcare APIs directly support clinical decision-making by connecting innovative user interfaces with underlying data systems. This connectivity enables more personalized care through comprehensive data aggregation, giving providers a complete picture of each patient's health journey.
When implemented effectively, APIs allow clinicians to access the right information at the right time, directly impacting treatment decisions and patient outcomes.
Improving Operational Efficiency
Beyond clinical applications, healthcare APIs dramatically improve operational efficiency by automating administrative tasks like appointment scheduling and medical billing. This automation reduces manual data entry requirements and minimizes errors, allowing healthcare staff to focus more on patient care rather than paperwork.
The operational benefits extend throughout healthcare organizations, from front-desk operations to back-office functions.
Essential Building Blocks: Core Functionality Every Healthcare API Needs
Healthcare APIs require specific functional capabilities to operate effectively in clinical environments. These foundational elements determine whether your API can handle the unique demands of healthcare data exchange.
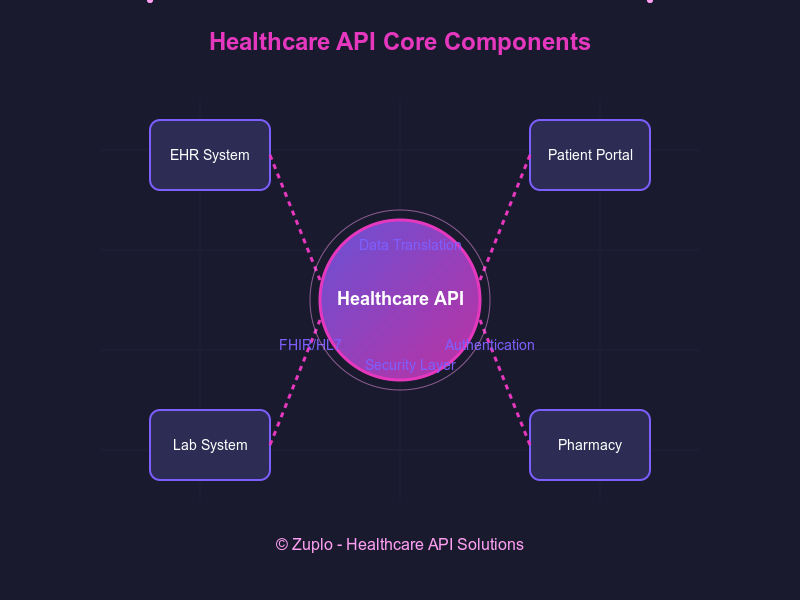
At their foundation, healthcare APIs must function effectively as data translators, converters, and system connectors. Understanding these core capabilities helps ensure your API implementation meets fundamental requirements for healthcare data exchange.
Data Translation Capabilities
Effective healthcare APIs must convert data between different formats (JSON, XML, and others) to enable cross-application communication. This translation capability creates a universal language between disparate systems, allowing them to exchange information regardless of how data is originally stored.
The translation layer must handle various data types while preserving the integrity and meaning of the information being exchanged.
Creating Seamless Data Exchange
Healthcare APIs facilitate data transfer between healthcare companies and other parties through a standardized request-response model. When information is needed, one system sends a request through the API, and the receiving system validates this request and returns the requested data.
This exchange mechanism must work reliably across organizational boundaries while maintaining appropriate security controls.
Connecting Previously Siloed Systems
Perhaps most importantly, APIs link previously isolated systems within healthcare organizations and connect external systems like pharmacies, laboratories, and insurance providers. This interconnection creates a cohesive healthcare data ecosystem where information flows naturally between systems that were never designed to communicate.
By building bridges between these islands of information, healthcare APIs enable a more integrated approach to both care delivery and business operations.
Critical Success Factors: Make-or-Break Considerations for Healthcare APIs
When building healthcare APIs, several crucial factors will determine whether your implementation thrives or struggles. These considerations address the most challenging aspects of healthcare data exchange and directly impact adoption rates among your target users.
When building healthcare APIs, several critical factors demand your attention. Let's tackle the most important considerations that will determine your API's success.
Interoperability Standards and Protocols
Interoperability remains the elephant in the room for healthcare technology. It's still one of healthcare's biggest headaches, and your API strategy needs to tackle this challenge head-on through smart implementation of industry standards.
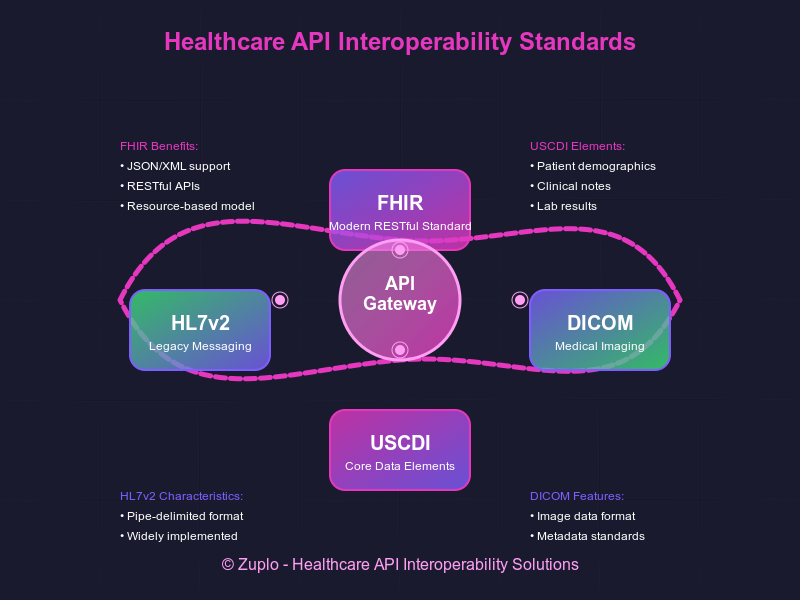
Embracing FHIR for Modern Healthcare Integration
The Fast Healthcare Interoperability Resources (FHIR) standard has emerged as the leading framework for healthcare data exchange. This RESTful API approach provides a common language for healthcare system communication, facilitating more straightforward integration between systems.
FHIR's resource-based model mirrors how healthcare professionals think about data, making it intuitive for developers who understand healthcare workflows.
Actionable Tip: Start with the FHIR core resources that align with your most critical use cases rather than trying to implement the entire standard at once. This incremental approach lets you deliver value quickly while building toward comprehensive implementation.
Supporting Legacy Standards
While FHIR represents the future, many healthcare organizations still rely on established standards like HL7v2 for clinical messaging and DICOM for medical imaging. Effective healthcare APIs often need to support these legacy protocols alongside newer standards.
This dual support creates bridges between established systems and more modern applications, preventing information silos from forming during transition periods.
Actionable Tip: Create abstraction layers that translate between legacy standards and modern API interfaces, allowing new applications to communicate with older systems without needing to understand outdated protocols.
Adhering to Core Data Standards
The United States Core Data for Interoperability (USCDI) defines essential data elements that should be exchangeable across systems. Aligning your API with these standards ensures you're capturing and transmitting the information most critical to healthcare operations.
Building these standards into your API design from the beginning is significantly easier than retrofitting them later, making this an important early consideration.
Actionable Tip: Map your existing data elements to USCDI standards, identifying gaps that need to be addressed. Prioritize these gaps based on clinical importance and frequency of use in information exchange.
Security and Compliance Considerations

Healthcare APIs unlock amazing possibilities for sharing data, but — and this is a big but — they also come with serious security and compliance responsibilities. As more healthcare organizations jump on the API bandwagon, they're quickly learning they need to navigate a maze of security requirements and regulatory frameworks.
Implementing Robust Authentication
Every healthcare API must implement strong authentication mechanisms to verify the identity of systems and users attempting to access sensitive information. OAuth 2.0 has become the industry standard for secure token-based authentication, providing a framework for controlling API access.
Beyond basic authentication, consider implementing multi-factor authentication for highly sensitive operations and risk-based authentication that adapts security requirements based on the context of each request.
Actionable Tip: Implement token expiration policies that balance security with user experience — shorter lifespans for tokens accessing highly sensitive data, longer lifespans for tokens with limited access rights, reducing authentication friction for common operations.
Protecting Data in Transit and at Rest
Healthcare APIs must protect patient data at every stage of its journey. This requires encrypting all Protected Health Information (PHI) both during transmission and when stored in databases or other systems.
Transport Layer Security (TLS) 1.2 or higher with strong cipher suites should be the minimum standard for all API communications, ensuring data cannot be intercepted during transmission between systems.
Actionable Tip: Conduct regular encryption key rotation and management reviews. Create an automated process that alerts you when certificates are approaching expiration, preventing unexpected downtime from expired security credentials.
Maintaining HIPAA Compliance
Healthcare APIs handling patient information must adhere to HIPAA requirements for protected health information. This includes implementing comprehensive risk management programs and maintaining vigilance to avoid violations that can result in substantial fines.
HIPAA compliance extends beyond technical controls to include administrative safeguards like staff training and operational procedures that govern how API access is managed within your organization.
Actionable Tip: Create role-based access templates aligned with common healthcare job functions, making it easier to assign appropriate permissions consistently across your organization while maintaining the principle of least privilege.
Implementing Comprehensive Audit Logging
Maintaining detailed records of all API interactions is essential for both security monitoring and regulatory compliance. Your logging system should capture who accessed what data, when they accessed it, and what actions they performed.
These audit trails are invaluable for investigating security incidents and demonstrating compliance during regulatory audits.
Actionable Tip: Build dashboards that visualize access patterns, helping you identify unusual behaviors that might indicate security issues. Set up automated alerts for access attempts that deviate from established patterns, like after-hours access or unusual data volume requests.
Speed and Reliability: Performance Strategies That Actually Work
In healthcare environments where seconds matter, API performance isn't just a technical metric—it's a clinical necessity. These optimization approaches address the unique performance challenges faced by healthcare systems handling sensitive patient information under time pressure.
API performance directly impacts both user experience and system reliability in healthcare environments. Implementing these optimization strategies can help your healthcare API handle the demands of modern healthcare operations.
Effective Caching Implementation
Strategic caching of API responses can dramatically improve performance for frequently requested data. By storing the results of expensive operations or commonly requested information, you can reduce database load and improve response times.
Consider implementing multiple caching layers, including edge caching through CDNs for public information and application-level caching for authenticated data, each optimized for different types of healthcare information.
Managing API Throughput
Healthcare APIs must handle varying loads, from routine daily traffic to sudden spikes during health emergencies. Implementing rate limiting creates sensible boundaries on requests so no single client can overwhelm your systems.
These limits should be designed to protect system stability while still ensuring critical healthcare information remains available when needed.
Optimizing Payload Size
Excessive payload sizes lead to slower response times and higher bandwidth consumption—both critical concerns in healthcare environments where timely data access can impact patient care. Consider implementing compression methods like Gzip for API responses while ensuring all transmitted data is relevant to the specific request.
GraphQL offers another approach by allowing selective data requests, keeping network usage lean while giving clients precisely the information they need.
Asynchronous Processing for Complex Operations
Not all healthcare operations need to happen synchronously. For resource-intensive tasks like processing large imaging studies or generating complex reports, asynchronous processing can dramatically improve API responsiveness.
Instead of making users wait while a time-consuming operation completes, your API can acknowledge the request and process it in the background, notifying the client when results are available.
Patient-Centered Design: How APIs Transform Care Delivery
While technical discussions often dominate API development, the ultimate purpose of healthcare APIs is improving patient care. These implementation approaches demonstrate how well-designed APIs directly enhance clinical outcomes and patient experiences.
The ultimate measure of healthcare API success is its impact on patient care. These are the ways effective API implementations are transforming healthcare delivery.
Creating Comprehensive Patient Profiles
By aggregating data from multiple sources, healthcare APIs enable the creation of complete patient profiles, giving providers access to medical histories, lab results, and imaging reports in one place. This comprehensive view allows for more personalized and informed care decisions.
The ability to access this complete picture regardless of where care was previously delivered represents a significant advancement in healthcare coordination.
Improving Care Coordination
Real-time data sharing through APIs facilitates better communication between providers across different care settings. This coordination reduces gaps in care and prevents duplicate tests and procedures, creating a more seamless experience for patients moving between providers.
APIs enable this coordination to happen automatically in the background without requiring direct communication between busy healthcare professionals.
Empowering Patient Engagement
API-powered patient portals and mobile apps provide easier access to health information, allowing patients to actively participate in their care. These tools transform patients from passive recipients of healthcare to engaged partners in managing their health.
The growing ecosystem of patient-facing applications built on healthcare APIs is creating new channels for patient-provider communication and health monitoring outside traditional clinical settings.
Accelerating Diagnosis and Treatment
APIs enable real-time access to lab results and diagnostic information, speeding up the time from testing to treatment decisions. AI-powered clinical decision support tools that leverage API data can further improve diagnostic accuracy and suggest evidence-based treatment options.
This acceleration of the diagnostic and treatment process directly impacts patient outcomes, particularly for time-sensitive conditions.
Overcoming Obstacles: Solutions to Common API Roadblocks
Despite their benefits, healthcare APIs face specific implementation challenges that can derail even the most promising projects. Understanding these obstacles and having strategies to address them can mean the difference between successful adoption and abandoned initiatives.
Despite their benefits, healthcare APIs face several implementation challenges that must be addressed for successful adoption.
Breaking Down Technical Barriers
Healthcare organizations often encounter technical hurdles when implementing APIs, including difficulties accessing API endpoints and limited access to testing environments. These challenges can significantly slow development and integration efforts.
Overcoming these barriers requires clear documentation, accessible testing environments, and responsive support channels for developers working with your API.
Managing Integration Costs
The financial aspects of API integration can present significant obstacles, with high fees often cited as a primary challenge to API adoption. These costs can create barriers to entry, particularly for smaller healthcare organizations and innovative startups.
A thoughtful approach to pricing and licensing can help make your healthcare API more accessible while still supporting sustainable development.
Navigating the Standardization Landscape
The lack of universally adopted API standards across healthcare creates integration challenges, with organizations often needing to support multiple standards and formats. This complexity increases development costs and complicates maintenance.
While standards like FHIR are gaining traction, the transition period requires flexible approaches that can work with various data formats and exchange protocols.
Ensuring Vendor Responsiveness
Healthcare organizations frequently report challenges with vendor responsiveness, particularly for smaller clients. This lack of support can significantly impede implementation efforts and ongoing operations.
Establishing clear service level agreements and support channels is essential for maintaining effective API operations in healthcare environments.
Looking Forward: Emerging Technologies Reshaping Healthcare APIs
The rapidly evolving healthcare technology landscape continues to create new opportunities and expectations for API capabilities. These emerging trends are already beginning to influence API development priorities and will likely become standard requirements in the near future.
The landscape of healthcare APIs continues to evolve rapidly, with several emerging trends set to shape future implementations.
AI and Machine Learning Integration
Healthcare APIs are increasingly serving as the foundation for AI-driven applications across the medical field. These integrations are especially notable in medical imaging, where APIs enable enhanced image analysis and provide robust diagnostic support.
As AI capabilities advance, APIs will play a crucial role in making these technologies accessible within existing healthcare workflows and systems.
Advancing Personalized Medicine
Healthcare APIs are central to the advancement of personalized medicine, facilitating customized treatment plans based on individual genetic profiles, lifestyle factors, and environmental considerations. The emerging use of APIs in genomics is creating unprecedented opportunities for precision healthcare.
These connections allow treatment recommendations to be tailored to individual patients, accounting for their unique health characteristics and potential responses to different interventions.
Edge Computing in Healthcare
By processing data closer to its origin rather than sending everything to centralized servers, edge computing is dramatically cutting latency for time-sensitive healthcare operations. This approach is particularly valuable for remote patient monitoring and urgent care scenarios.
Healthcare APIs that support edge computing models can deliver near-immediate responses for critical applications while reducing bandwidth requirements for data-intensive healthcare monitoring.
Expanding Remote Care Capabilities
The rapid growth of telemedicine has been supported by API implementations that connect virtual care platforms with Electronic Health Records. These integrations enable secure data access during virtual appointments and allow providers to update records seamlessly after telehealth consultations.
As remote care continues to expand, APIs will become even more critical for maintaining continuity between virtual and in-person care delivery.
Implementation Playbook: Best Practices for Healthcare API Success
Successful healthcare API implementation requires balancing technical excellence with healthcare's unique requirements. These field-tested best practices come from organizations that have navigated the challenges and built APIs that deliver real clinical and operational value.
Successful healthcare API implementation requires attention to several key best practices throughout the development and deployment process.
Designing for Developer Experience
Well-designed healthcare APIs are easier to integrate and maintain. Follow REST architectural principles, including standard HTTP methods and proper resource naming. Generate interactive API documentation using tools like Swagger or Redoc to help developers quickly understand how to use your API.
Including detailed descriptions of endpoints, parameters, and responses with code samples dramatically reduces the learning curve for developers working with your healthcare API.
Implementing Proper Versioning
Healthcare APIs evolve over time, but changes can disrupt existing integrations. Implement versioning (URL or header-based) to support backward compatibility and communicate deprecation timelines for older API versions.
This approach allows systems using your API to update at their own pace while ensuring everyone eventually moves to newer, more secure versions.
Planning for Scale
Healthcare data volumes continue to grow exponentially, and your API must be able to scale accordingly. Ensure your API infrastructure can handle increasing request volumes without performance degradation, and implement caching mechanisms to improve performance under heavy load.
Consider asynchronous processing for time-consuming operations to maintain responsiveness even during peak usage periods.
Preparing for the Unexpected
Healthcare operations cannot tolerate extended downtime. Use standardized error responses with meaningful error codes that don't expose sensitive information, and implement proper logging for troubleshooting and auditing.
Have backup API providers or failover mechanisms in place, and regularly test disaster recovery plans to ensure you can maintain operations during system failures or other emergencies.
Building the Connected Healthcare Ecosystem
Healthcare APIs have evolved beyond optional technical components to become the essential backbone of modern healthcare systems. When you master the fundamentals that we cover here — security that actually protects patient data, true interoperability, lightning-fast performance, and interfaces developers won't hate using — you're not just checking boxes, you're setting up systems that deliver better care, streamlining operations, and enabling innovations that seemed impossible just a few years ago.
Ready to level up your healthcare systems? Zuplo makes building, deploying, and managing healthcare APIs dramatically simpler with developer-friendly tools that don't sacrifice compliance. Our built-in security features and performance optimization mean you can focus on creating value, not wrestling with infrastructure. Create a Zuplo account today and start building the connected healthcare systems your organization (and patients) deserve.